Abstract
Purpose
Pseudomyxoma peritonei (PMP) is a rare clinical malignancy syndrome characterized by the uncontrollable accumulation of copious mucinous ascites in the peritoneal cavity, resulting in “jelly belly”. The mechanism of tumor progression and mucin hypersecretion remains largely unknown, but GNAS mutation is a promising contributor. This review is to systemically summarize the biological background and variant features of GNAS, as well as the impacts of GNAS mutations on mucin expression, tumor cell proliferation, clinical-pathological characteristics, and prognosis of PMP.
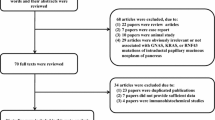
Methods
NCBI PubMed database (in English) and WAN FANG DATA (in Chinese) were used for literature search. And NCBI Gene and Protein databases, Ensembl Genome Browser, COSMIC, UniProt, and RCSB PDB database were used for gene and protein review.
Results
GNAS encodes guanine nucleotide-binding protein α subunit (Gsα). The mutation sites of GNAS mutation in PMP are relatively stable, usually at Chr20: 57,484,420 (base pair: C-G) and Chr20: 57,484,421 (base pair: G-C). Typical GNAS mutation results in the reduction of GTP enzyme activity in Gsα, causing failure to hydrolyze GTP and release phosphoric acid, and eventually the continuous binding of GTP to Gsα. The activated Gsα could thus continuously promote mucin secretion through stimulating the cAMP-PKA signaling pathway, which is a possible mechanism leading to elevated mucin secretion in PMP.
Conclusion
GNAS mutation is one of the most important molecular biological features in PMP, with major functions to promote mucin hypersecretion.
Similar content being viewed by others
Introduction
Pseudomyxoma peritonei (PMP) is a rare clinical malignancy syndrome usually caused by the perforation of appendiceal mucinous tumor and the “redistribution phenomenon” of mucus and tumor cells, with an incidence of 1–2/million (Mittal et al. 2017; Smeenk et al. 2008). PMP is characterized by a large volume of mucinous ascites, multiple peritoneal implantations, omental cake, and ovarian involvement in women macroscopically, and abundant mucus pools microscopically. The chronic and uncontrollable mucus accumulation is one of the major clinical features of PMP (O’Connell et al. 2002a, b), which gradually leads to intraperitoneal organ adhesion, bowel obstruction, malnutrition, and eventually cachexia and death. Aggressive cytoreductive surgery (CRS) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) could bring significant survival benefit to PMP (Chua et al. 2012; Li et al. 2018), and has been recommended by Peritoneal Surface Oncology Group International (PSOGI) as the standard treatment of PMP (Li et al. 2014, 2019).
Although treated with CRS plus HIPEC, patients frequently suffered from relapse, presenting aggravated “jelly belly”. One of the difficulties in studying PMP is the scarcity of knowledge in the fundamental molecular mechanisms underlying mucus hypersecretion. It has been reported that Kirsten rat sarcoma viral oncogene homolog (KRAS) and guanine nucleotide-binding protein alpha subunit (GNAS) are two of the most frequently detected variants in PMP, and GNAS mutation plays an important role in the regulation of mucin expression (Bradbury 2000; Jarry et al. 1994; Nishikawa et al. 2013). To have a better insight into the role of GNAS gene in PMP, we systemically reviewed the biological background of GNAS, current studies concerning the variant feature of GNAS, the impacts of GNAS mutations on mucin expression, tumor cell proliferation, and clinical–pathological characteristics and prognosis.
The biological background of GNAS gene
Basic structure and function
The GNAS gene is located at chromosome 20q13.32 (chromosome 20: 57,414,773–57,486,247), which also names GNAS complex locus (Fig. 1a), consisting of 13 exons and 12 introns. GNAS is responsible for the encoding of stimulatory guanine nucleotide-binding protein (G protein) α subunit (Gsα), which transduces signals from G protein-coupled receptors (GPCR) to adenyl cyclase (AC), and finally regulates the expression of cyclic adenosine monophosphate (cAMP).
The location and biological structure of GNAS gene. aGNAS gene is located at chromosome 20q13.32; b thirteen exons and the upstream alternative first exons of GNAS. The imprinted expression pattern of GNAS is highly complicated, with exclusively maternal expression of NESP55 (red arrow), and exclusively paternal expression of NESPAS, XL exon and exon 1A (green arrow). NESPAS: NESP anti sense
DNA transcription and translation
The promoter region of Gsα is located at the CpG island upstream of exon 1, which is usually unmethylated in alleles of both parental origins (Bird 1986; Gardiner-Garden and Frommer 1987). It was reported by Mantovani et al. (2002) and Germain-Lee et al. (2005) that Gsα imprinted with tissue-specific pattern in kidney cortex, thyroid gland, pituitary gland, and ovary, which is mainly maternally expressed. There are four kinds of alternative promoter regions upstream of Gsα exon 1 (Weinstein et al. 2001): (1) promoter 1, about 49 kb upstream of Gsα exon 1, encodes neuroendocrine secretory protein 55 (NESP55). The coding sequence is within the upstream of Gsα exon 1, leaving exon 2–13 untranslated region; (2) promoter 2, about 2–3 kb upstream of XL exon, initiates NESP55 exon transcription from the opposite direction; (3) promoter 3, about 35 kb upstream of Gsα exon 1, encodes extra-large alphas protein (XLαs), whose coding sequence is composed of XL exon and Gsα exon 1; (4) promoter 4 locates at about 2.5 kb upstream of Gsα exon 1. The resulted exon 1A transcripts were presumed to be untranslated mRNAs. The imprinted expression patterns of the aforementioned promoters are highly complicated. NESP55 is maternally expressed, while NESP anti sense, XLαs, and exon 1A are paternally expressed (Fig. 1b) (Crane et al. 2009).
The UniProt database (https://www.uniprot.org/) was used to search for proteins encoded by GNAS, with the searching term as “gene: GNAS AND reviewed: yes AND organism: “Homo sapiens (Human) [9606]””. The result showed four kinds of proteins encoded by GNAS: (1) Gsα, with a length of 394 amino acid residues, is encoded by GNAS exon 1–13; (2) XLαs, with a length of 1037 amino acid residues, is paternally expressed and responsible for the stimulation of AC-cAMP–PKA signaling pathway. XLαs is one of the isoforms of Gsα, with similar downstream receptor to Gsα. But there is no evidence showing that seven-transmembrane receptors activating Gsα can also activate XLαs; (3) protein ALEX, with a length of 626 amino acid residues, is the product of paternal expression of XL exon and possibly contributes to the inhibition of AC activity in XLαs subunit (Abramowitz et al. 2004); (4) NESP55, with a length of 245 amino acids, is maternally expressed and encoded by NESP55 exon. NESP55 forms LHAL tetrapeptide and GPIPIRRH peptide after modification and shear.
The structure and function of Gsα
Among the four reviewed proteins, Gsα is the main product of GNAS gene, which includes two domains (Rose et al. 2018) (Fig. 2). The first is guanosine triphosphate enzyme (GTPase) domain, which is formed after the fold of 39–394th amino acid residues. GTPase domain functions as the guanosine-biding and interaction site for receptors and effectors. There are four guanosine triphosphate/guanosine diphosphate (GTP/GDP)-binding sites, located at 47–55th, 197–204th, 223–227th, and 292–295th amino acid residues respectively; and two magnesium ion-binding sites, located at 54th and 204th amino acid residues, respectively. Two out of the four GTP/GDP-binding sites are highly conserved [arginine201 (Arg201) and glutamine227 (Gln227)], which play a vital role on the hydrolysis of the bound GTP. The second is helical domain, with a possible function of maintaining the binding status between GTP/GDP and Gsα (Weinstein et al. 2001). Besides the four domains, there are five motif structures in Gsα, including G1 (42–55th amino acids), G2 (196–204th amino acids), G3 (219–228th amino acids), G4 (288–295th amino acids), and G5 (364–369th amino acids).
The tertiary structure of Gsα subunit (cited from RCSB PDB database, https://www.rcsb.org/; PDB ID: 6AU6). Magenta and purple: α-helix; yellow and blue: β-sheet; white: random coil. Arg arginine, Gln glutamine, GTP guanosine triphosphate, GTPase GTP enzyme, GDP guanosine diphosphate
The signaling from GPCR to the downstream molecules is carried out through G protein cycle (Fig. 3, red-dotted box): (1) Gsα releases GDP and combines with GTP due to the affinity reduction between Gsα and GDP caused by activation from ligand-binding GPCR to Gsα; (2) GTP-binding Gsα separates with β and γ subunits and turns into an activated status, which is able to stimulate downstream molecules; (3) as reacting with the downstream molecules, the GTPase activity of Gsα is activated and then GTP is hydrolyzed. Eventually, Gsα returns to the primary structure and reforms trimer with β and γ subunits.
G protein cycle, activity changes of Gsα subunit caused by GNAS mutation, and the crosslink among Gsα subunit-induced cAMP–PKA, PI3K–Akt, and RAS–MAPK pathways. Red dotted box: G protein cycle; blue dotted box: activity changes of Gsα subunit caused by the mutation of Gsα Arg201. ① In the physiological status, activated Gsα returns to deactivated status after releasing a Pi; ② In the situation of Arg201 mutation, Gsα fails to release Pi and remains in activated status. Gsα in ink blue: deactivated status. Gsα in light blue: activated status; the other signaling pathways: cAMP–PKA, PI3K–Akt, and RAS–MAPK pathways interacts among each other and eventually modulate mucin gene expression via the nuclear import of ATF/CREB and NFκB. GPCR G protein-coupled receptor, Gsα stimulatory G protein subunit, Pi inorganic phosphate, AC adenyl cyclase, cAMP cyclic adenosine monophosphate, PKA protein kinase A, ATF activating transcription factor, CREB cAMP-response element-binding protein, PLC phospholipase C, PKC protein kinase C, PI3K phosphoinositide 3-kinase, Akt protein kinase B, PDE4B phosphodiesterase 4B, RTK receptor tyrosine kinases, Ras rat sarcoma protein, Raf-1 Raf-1 protein, P42MAPK P42 mitogen-activated protein kinas, also named Erk2, extracellular signal-regulated kinase 2, PP90rsk 90 kDa ribosomal S6 kinase, NFκB nuclear factor kappa-light-chain-enhancer of activated B cells, Sp1 specificity protein 1, Arg arginine, Cys cysteine, His histidine
The molecular changes of GNAS mutation
A thorough literature research identified 13 papers reporting the genetic variants and corresponding gene mutation rates in PMP. Only variants reported in ≥ 5 papers were listed in Table 1. As listed in Table 1, the two most frequent variants in PMP are KRAS and GNAS mutations, with a median mutation rates of 77.8% (range 40.0–100%) and 45.7% (range 25.7–100%) respectively. By reviewing papers describing the detailed variant form of GNAS, we found that the most frequently detected GNAS mutation forms were c.602G>A (p.R201H) and c.601C>T (p.R201C) (Table 2). Despite the different variant forms reported by Pengelly et al. (2018) and Saarinen et al. (2017), the variant sites were relatively stable, both located at Chr20: 57,484,420 and Chr20: 57,484,421, which was identical to c.602G>A (p.R201H) and c.601C>T (p.R201C). Various transcripts chosen after sequencing might have resulted in the different expression patterns of mutation sites. Thus, it can be concluded that Chr20: 57,484,420 C>T (c.601C>T: p.R201C) and Chr20: 57,484,421 G>A (c.602G>A: p.R201H) are the two most significant variant forms in PMP GNAS mutations.
Taking the encoding of Gsα for example, once c.601C>T and c.602G>A mutation occur, the 201th amino acid residue, Arg, changes into cysteine (Cys) and histidine (His) respectively. The variants significantly alter the structure of GTPase domain in Gsα, and vastly decrease GTPase activity. As a consequence, Gsα fails to hydrolyze GTP and release phosphoric acid, remaining in activated status, which continuously stimulates downstream molecules (Fig. 3, blue dotted box).
Influences of GNAS mutation to mucin secretion and cell proliferation
Mucin expression in PMP
There are two major types of mucins, gel-forming mucins and transmembrane mucins (Johansson and Hansson 2016). Gel-forming mucins mainly include MUC2, MUC5AC, MUC5B, and MUC6. Transmembrane mucins mainly consist of MUC1, MUC3, MUC4, MUC12, MUC13, MUC16, and MUC17. A thorough review of the published literatures on mucin expression in PMP identified some distinctive features (Table 3). First, most researches focus on the expression status of gel-forming mucins, while little attention has been paid to transmembrane mucins. Second, MUC2 and MUC5AC are the most frequently expressed gel-forming mucins in PMP, with positive rates being 99.1% (314/317) and 96.5% (193/200), respectively, among the detected samples. MUC6 is rarely detected in PMP compared with MUC2 and MUC5AC, with positive rate of 12.5% (2/16). Third, the transmembrane MUC1 expresses variably in PMP, with positive rate being 41.3% (33/80). The expression status of MUC4 is currently unclear due to the limitation of sample number. Based on the available data from published literatures, it is advisable to focus more attention on in-depth study on MUC2 and MUC5AC.
GNAS functions on the regulation of mucin secretion
GNAS mutation is frequently detected in mucinous neoplasms of appendix (50%) and intraductal papillary mucinous neoplasm (IPMN) of pancreas (81%) (Furukawa et al. 2011; Wu et al. 2011), while the mutation rate in mucinous adenocarcinoma of colorectum, ovary, lung, and breast are relatively lower, even being 0% (Nishikawa et al. 2013). In addition, both PMP and IPMN share similar inertia biological behavior as well as hypersecretion of mucus. Therefore, it is inferred that GNAS might play some role in the regulation of mucin secretion (Alakus et al. 2014; Noguchi et al. 2015; Tokunaga et al. 2019).
The effect of GNAS mutation to mucin secretion has been proved by Nishikawa et al. (2013). The author transfected HT29 cells with an EF1a-GNASR201H-IRES-Zeo plasmid. The result showed that cAMP, MUC2, and MUC5AC level elevated after the expression of GNASR201H. While the application of PKA inhibitor downregulated the expression of MUC2 and MUC5AC genes. Nishikawa’s study demonstrates that GNAS mutation might regulate mucin production through cAMP–PKA signaling pathway (Bradbury 2000; Jarry et al. 1994). The potential regulation method of cAMP–PKA signaling pathway might be stimulating cAMP-response element-binding protein (CREB) and activating transcription factor (ATF) family (Velcich and Augenlicht 1993). After entering nucleus, the activated CREB/ATF combines to the upstream cis-acting element of mucin genes and thus regulate mucin expression. Other studies have also proved that inhibitors of both PKA and heterotrimer G protein complex could also significantly downregulate mucin expression. Although GNAS mutation is proved to be an important promoter in mucin secretion of PMP, the current experiment was performed in colorectal cancer cell lines due to the difficulties in the culture of PMP tumor cells (Nishikawa et al. 2013). Besides, the influence of GNAS mutation to different types of mucin still needs further exploration.
The existed pathways which have cross reaction with cAMP–PKA pathway also participate in the regulation of mucin expression indirectly (Fig. 3): (1) MAPK signaling pathway. The activated cAMP influences MAPK signaling pathway via activating Ras or inhibiting Raf-1 by PKA. In pulmonary cystic fibrosis, it has been illustrated that hyperexpression of MUC2 was mainly regulated through Src/Ras/MAPK/pp90rsk signaling pathway (Li et al. 1998). However, the function of Src/Ras/MAPK/pp90rsk in PMP is not proven currently; (2) Ras–PI3K–Akt signaling pathway. PDE4B activated by this pathway functions as an antagonist against cAMP–PKA signaling pathway by clearing cAMP (Alakus et al. 2014); (3) PKC signaling pathway. Activated PKC has synergistic effect on cAMP–PKA pathway through activating Raf-1. Besides, Ca2+-dependent PKC-epsilon could also upregulate MUC2 and MUC5AC expression (Hong et al. 1999).
GNAS functions on the regulation of tumor cell proliferation
Generally, the current studies support the notion that PMP and colorectal cancer share similar gene mutation profiles, but vary vastly in mutation rate. PMP possesses higher mutation rates in GNAS and KRAS, while lower mutation rates in TP53, APC, and PIK3CA (Alakus et al. 2014; Tokunaga et al. 2019). Nishikawa et al. transfected HT29 cells with an EF1a-GNASR201H-IRES-Zeo plasmid. The cell proliferation remained the same, but accompanied with elevated mucin secretion. The result indicated that GNAS mutation mainly affect the expression level of mucin instead of tumor cell proliferation. KRAS is another important variant in PMP, and has been reported to promote tumor cell proliferation through the activation of MAPK signaling pathway (Alakus et al. 2014; Pylayeva-Gupta et al. 2011).
Impacts of GNAS mutation to clinical–pathological characteristics and prognosis
Correlation of GNAS mutation and clinical–pathological characteristics
In a study cohort of 55 patients, Singhi et al. (2014) demonstrated no significant association between GNAS mutation and gender, age, and adverse histological features (including cytologic grade, destructive invasion, tumor cellularity, angiolymphatic invasion, perineural invasion, and signet ring cells) (P > 0.05). However, the author found that GNAS-mutated PMP was prone to harbor concurrent KRAS mutation compared with GNAS-wild-type PMP (65% vs. 29%, P = 0.018).
Pietrantonio et al. (2016a, b) analyzed 15 patients with relapsed PMP, and revealed no association between GNAS mutation and gender, age, Eastern Cooperative Oncology Group performance status, histological grade, time elapsed from surgery to relapse, peritoneal cancer index (PCI), and completeness of cytoreduction. In another study of 40 PMP patients, Pietrantonio et al. (2016a, b) found that GNAS mutation was correlated to incomplete cytoreduction (P = 0.05) and KRAS mutation (P = 0.002). Besides, neither GNAS nor KRAS mutation were associated with pathological grade (P = 0.338 and 0.427, respectively).
From the studies by Pietrantonio et al. (2016a, b) and Singhi et al. (2014), it could be inferred that the presence of GNAS mutation is related to KRAS mutation. Considering the high incidence of these two variants in PMP and the statistically close relationship, the independent and synergistic effect as wells as the crosslink between GNAS and KRAS could be important issues to be explored in the mechanical studies of PMP.
Despite of the application of different criteria in histopathological classification, most of the studies showed that GNAS mutational status had no association with histopathological grade (Gleeson et al. 2018; Nummela et al. 2015; Pietrantonio et al. 2016a, b; Singhi et al. 2014). However, opposite opinions existed concerning the relation between GNAS mutation and histopathological grade. Noguchi et al. (2015) investigated mutation profiles of 18 PMP patients, revealing GNAS mutation in five low-grade PMP and three high-grade PMP. Noguchi hold the view that GNAS mutation might play a key role in both low-grade and high-grade PMP. On the contrast, in a study performed by Alakus et al. (Alakus et al. 2014), the result revealed that GNAS mutation rate is lower in high-grade PMP (21/23 vs. 1/6, P = 0.005). For the only patient with high-grade PMP presenting GNAS mutation, it was observed that the histopathology of the intraperitoneal implantation was a mixture of partly low-grade and partly high-grade PMP. Considering the existence of low-grade loci, Alakus et al. made a conclusion that high-grade PMP might not evolve from low-grade PMP.
Impacts of GNAS mutation on PMP prognosis
Few studies were performed to investigate the association between GNAS mutation and prognosis of PMP. The results varied among different studies. Singhi et al. (2014) found that GNAS mutation did not affect the overall survival (OS) or time to disease progression. High tumor grade (AJCC G2 and G3) (P = 0.002) and lymph node involvement (P = 0.025) were associated with poorer OS. While HIPEC was associated with improved OS. Cox proportional hazard model identified that only lymph node involvement was the independent prognostic factor of PMP. In a study performed by Pietrantonio et al. (2016a, b), it was found that patients with GNAS mutation had significantly shorter median progression-free survival (PFS) than GNAS-wild type patients (5.3 months vs. not reached, P < 0.007). Later, in a study cohort of 40 patients, Pietrantonio et al. again demonstrated that GNAS mutation was associated with PFS. The other variables correlated to PFS were completeness of cytoreduction score, PCI score, and KRAS mutation status. However, multiple variate analysis revealed only PCI > 20 and KRAS mutation were the independent predictors of PFS.
Summary
To sum up, GNAS mutation is one of the most important molecular biological features in PMP, which might function as promoting the secretion of mucin. The mutation sites of GNAS mutation is relatively stable, usually at Chr20: 57,484,420 (base pair: C-G) and Chr20: 57,484,421 (base pair: G-C). The presence of GNAS mutation results in the reduction of GTPase activity in Gsα, causing failure to hydrolyze GTP and release phosphoric acid, and eventually the continuous combining status of Gsα and GTP. The activated Gsα could thus continuously stimulate mucin secretion through the stimulation of cAMP–PKA signaling pathway. As presented above, there were already several studies proving that GNAS could elevate secretion level of mucin, but the experiments were limited in the cell lines of colorectal cancer. A more reliable evidence provided by experiments of genetic and protein level in PMP cell line is in urgent requirement.
The high mutation rate of GNAS in PMP patients has been observed about 10 years ago, when fresh tumor tissue or formalin-fixed, paraffin-embedded tissue was used for variant detection. However, the number of patients was limited, and most of the sequencings were non-whole-exome sequencing, which indicated the deficiency on the comprehensive view of PMP mutation profile. Generally speaking, the establishment of stable PMP cell line combined with comprehensive mutation profile would vastly help to improve the understanding of PMP genetically, and uncover the mechanism of PMP, especially the influence of GNAS mutation to mucin hypersecretion, which might eventually facilitate the innovation of new drugs targeting the molecules in the GNAS-related signaling pathways.
Availability of data and material
All data and material generated or used during the study are available from the corresponding author by request.
References
Abramowitz J, Grenet D, Birnbaumer M, Torres HN, Birnbaumer L (2004) XLalphas, the extra-long form of the alpha-subunit of the Gs G protein, is significantly longer than suspected, and so is its companion Alex. Proc Natl Acad Sci USA 101:8366–8371
Alakus H et al (2014) Genome-wide mutational landscape of mucinous carcinomatosis peritonei of appendiceal origin. Genome Med 6:43. https://doi.org/10.1186/gm559
Bibi R, Pranesh N, Saunders MP, Wilson MS, O'Dwyer ST, Stern PL, Renehan AG (2006) A specific cadherin phenotype may characterise the disseminating yet non-metastatic behaviour of pseudomyxoma peritonei. Br J Cancer 95:1258–1264. https://doi.org/10.1038/sj.bjc.6603398
Bird AP (1986) CpG-rich islands and the function of DNA methylation. Nature 321:209–213. https://doi.org/10.1038/321209a0
Borazanci E, Millis SZ, Kimbrough J, Doll N, Von Hoff D, Ramanathan RK (2017) Potential actionable targets in appendiceal cancer detected by immunohistochemistry, fluorescent in situ hybridization, and mutational analysis. J Gastrointest Oncol 8:164–172. https://doi.org/10.21037/jgo.2017.01.14
Bradbury NA (2000) Protein kinase-A-mediated secretion of mucin from human colonic epithelial cells. J Cell Physiol 185:408–415. https://doi.org/10.1002/1097-4652(200012)185:3<408:AID-JCP11>3.0.CO;2-2
Chua TC et al (2012) Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol 30:2449–2456. https://doi.org/10.1200/JCO.2011.39.7166
Crane JL, Shamblott MJ, Axelman J, Hsu S, Levine MA, Germain-Lee EL (2009) Imprinting status of Galpha(s), NESP55, and XLalphas in cell cultures derived from human embryonic germ cells: GNAS imprinting in human embryonic germ cells. Clin Transl Sci 2:355–360. https://doi.org/10.1111/j.1752-8062.2009.00148.x
Ferreira CR, Carvalho JP, Soares FA, Siqueira SAC, Carvalho FM (2008) Mucinous ovarian tumors associated with pseudomyxoma peritonei of adenomucinosis type: immunohistochemical evidence that they are secondary tumors. Int J Gynecol Cancer 18:59–65. https://doi.org/10.1111/j.1525-1438.2007.00988.x
Flatmark K, Davidson B, Kristian A, Stavnes HT, Forsund M, Reed W (2010) Exploring the peritoneal surface malignancy phenotype—a pilot immunohistochemical study of human pseudomyxoma peritonei and derived animal models. Hum Pathol 41:1109–1119. https://doi.org/10.1016/j.humpath.2009.12.013
Furukawa T et al (2011) Whole-exome sequencing uncovers frequent GNAS mutations in intraductal papillary mucinous neoplasms of the pancreas. Sci Rep 1:161. https://doi.org/10.1038/srep00161
Gardiner-Garden M, Frommer M (1987) CpG islands in vertebrate genomes. J Mol Biol 196:261–282. https://doi.org/10.1016/0022-2836(87)90689-9
Germain-Lee EL et al (2005) A mouse model of albright hereditary osteodystrophy generated by targeted disruption of exon 1 of the Gnas gene. Endocrinology 146:4697–4709. https://doi.org/10.1210/en.2005-0681
Gleeson EM et al (2018) Appendix-derived pseudomyxoma peritonei (PMP): molecular profiling toward treatment of a rare malignancy. Am J Clin Oncol 41:777–783. https://doi.org/10.1097/coc.0000000000000376
Guo AT, Song X, Wei LX, Zhao P (2011) Histological origin of pseudomyxoma peritonei in Chinese women: clinicopathology and immunohistochemistry. World J Gastroenterol 17:3531–3537. https://doi.org/10.3748/wjg.v17.i30.3531
Heiskala K, Giles-Komar J, Heiskala M, Andersson LC (2006) High expression of RELP (Reg IV) in neoplastic goblet cells of appendiceal mucinous cystadenoma and pseudomyxoma peritonei. Virchows Arch 448:295–300. https://doi.org/10.1007/s00428-005-0105-1
Hong DH, Petrovics G, Anderson WB, Forstner J, Forstner G (1999) Induction of mucin gene expression in human colonic cell lines by PMA is dependent on PKC-epsilon. Am J Physiol 277:G1041–1047. https://doi.org/10.1152/ajpgi.1999.277.5.G1041
Jarry A, Merlin D, Hopfer U, Laboisse CL (1994) Cyclic AMP-induced mucin exocytosis is independent of Cl-movements in human colonic epithelial cells (HT29-Cl.16E). Biochem J 304:675–678
Johansson ME, Hansson GC (2016) Immunological aspects of intestinal mucus and mucins. Nat Rev Immunol 16:639–649. https://doi.org/10.1038/nri.2016.88
Li JD, Feng W, Gallup M, Kim JH, Gum J, Kim Y, Basbaum C (1998) Activation of NF-kappaB via a Src-dependent Ras–MAPK–pp90rsk pathway is required for Pseudomonas aeruginosa-induced mucin overproduction in epithelial cells. Proc Natl Acad Sci USA 95:5718–5723
Li Y, Yu Y, Liu Y (2014) Report on the 9(th) international congress on peritoneal surface malignancies. Cancer Biol Med 11:281–284. https://doi.org/10.7497/j.issn.2095-3941.2014.04.008
Li F, Qi CH, Lu YY, Hou F, Hao ZH, Zhai XC, Pang SJ (2017a) High-grade appendiceal mucinous neoplasm associated with pseudomyxoma peritonei: a clinicalpathologic analysis of 9 cases. J Diag Pathol 24(406–410):422
Li F, Qi CH, Lu YY, Hou F, Hao ZH, Zhai XC, Pang SJ (2017b) Pseudomyxoma peritonei of non-appendiceal origin: a clinicalpathologic analysis of eight cases. J Diag Pathol 24:86–91
Li XB, Lin YL, Ji ZH, Li Y (2018) Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy in patients with pseudomyxoma peritonei: analysis of 182 patients at a single center. Chin J Clin Oncol 45:943–949
Li Y, Xu HB, Peng Z, Cui SZ, Wu W (2019) Chinese expert consensus on cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for pseudomyxoma peritonei. Natl Med J China 99:1527–1535
Liu X et al (2014) Molecular profiling of appendiceal epithelial tumors using massively parallel sequencing to identify somatic mutations. Clin Chem 60:1004–1011. https://doi.org/10.1373/clinchem.2014.225565
Mantovani G, Ballare E, Giammona E, Beck-Peccoz P, Spada A (2002) The gsalpha gene: predominant maternal origin of transcription in human thyroid gland and gonads. J Clin Endocrinol Metab 87:4736–4740. https://doi.org/10.1210/jc.2002-020183
McKenney JK, Longacre TA (2008) Low-grade mucinous epithelial neoplasm (intestinal type) arising in a mature sacrococcygeal teratoma with late recurrence as pseudomyxoma peritonei. Hum Pathol 39:629–632. https://doi.org/10.1016/j.humpath.2007.08.021
Mittal R, Chandramohan A, Moran B (2017) Pseudomyxoma peritonei: natural history and treatment. Int J Hyperth 33:511–519. https://doi.org/10.1080/02656736.2017.1310938
Mohamed F, Gething S, Haiba M, Brun EA, Sugarbaker PH (2004) Clinically aggressive pseudomyxoma peritonei: a variant of a histologically indolent process. J Surg Oncol 86:10–15. https://doi.org/10.1002/jso.20038
Nishikawa G et al (2013) Frequent GNAS mutations in low-grade appendiceal mucinous neoplasms. Br J Cancer 108:951–958. https://doi.org/10.1038/bjc.2013.47
Noguchi R et al (2015) Molecular profiles of high-grade and low-grade pseudomyxoma peritonei. Cancer Med 4:1809–1816. https://doi.org/10.1002/cam4.542
Nonaka D, Kusamura S, Baratti D, Casali P, Younan R, Deraco M (2006) CDX-2 expression in pseudomyxoma peritonei: a clinicopathological study of 42 cases. Histopathology 49:381–387. https://doi.org/10.1111/j.1365-2559.2006.02512.x
Nummela P et al (2015) Genomic profile of pseudomyxoma peritonei analyzed using next-generation sequencing and immunohistochemistry. Int J Cancer 136:E282–289. https://doi.org/10.1002/ijc.29245
O’Connell JT, Hacker CM, Barsky SH (2002a) MUC2 is a molecular marker for pseudomyxoma peritonei. Mod Pathol 15:958–972. https://doi.org/10.1097/01.Mp.0000026617.52466.9f
O’Connell JT, Tomlinson JS, Roberts AA, McGonigle KF, Barsky SH (2002b) Pseudomyxoma peritonei is a disease of MUC2-expressing goblet cells. Am J Pathol 161:551–564. https://doi.org/10.1016/s0002-9440(10)64211-3
Pengelly RJ et al (2018) Analysis of mutation and loss of heterozygosity by whole-exome sequencing yields insights into pseudomyxoma peritonei. J Mol Diagn JMD 20:635–642. https://doi.org/10.1016/j.jmoldx.2018.05.002
Pietrantonio F et al (2016a) GNAS mutations as prognostic biomarker in patients with relapsed peritoneal pseudomyxoma receiving metronomic capecitabine and bevacizumab: a clinical and translational study. J Transl Med 14:125. https://doi.org/10.1186/s12967-016-0877-x
Pietrantonio F et al (2016b) Toward the molecular dissection of peritoneal pseudomyxoma. Ann Oncol 27:2097–2103. https://doi.org/10.1093/annonc/mdw314
Pylayeva-Gupta Y, Grabocka E, Bar-Sagi D (2011) RAS oncogenes: weaving a tumorigenic web. Nat Rev Cancer 11:761–774. https://doi.org/10.1038/nrc3106
Rose AS, Bradley AR, Valasatava Y, Duarte JM, Prlic A, Rose PW (2018) NGL viewer: web-based molecular graphics for large complexes. Bioinformatics 34:3755–3758. https://doi.org/10.1093/bioinformatics/bty419
Saarinen L et al (2017) Multiple components of PKA and TGF-beta pathways are mutated in pseudomyxoma peritonei. PLoS ONE 12:e0174898. https://doi.org/10.1371/journal.pone.0174898
Semino-Mora C, Liu H, McAvoy T, Nieroda C, Studeman K, Sardi A, Dubois A (2008) Pseudomyxoma peritonei: is disease progression related to microbial agents? A study of bacteria, MUC2 AND MUC5AC expression in disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis. Ann Surg Oncol 15:1414–1423. https://doi.org/10.1245/s10434-007-9778-9
Singhi AD et al (2014) GNAS is frequently mutated in both low-grade and high-grade disseminated appendiceal mucinous neoplasms but does not affect survival. Hum Pathol 45:1737–1743. https://doi.org/10.1016/j.humpath.2014.04.018
Sio TT, Mansfield AS, Grotz TE, Graham RP, Molina JR, Que FG, Miller RC (2014) Concurrent MCL1 and JUN amplification in pseudomyxoma peritonei: a comprehensive genetic profiling and survival analysis. J Hum Genet 59:124–128. https://doi.org/10.1038/jhg.2013.132
Smeenk RM, van Velthuysen ML, Verwaal VJ, Zoetmulder FA (2008) Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur J Surg Oncol 34:196–201. https://doi.org/10.1016/j.ejso.2007.04.002
Tokunaga R et al (2019) Molecular profiling of appendiceal adenocarcinoma and comparison with right-sided and left-sided colorectal cancer. Clin Cancer Res. https://doi.org/10.1158/1078-0432.Ccr-18-3388
Velcich A, Augenlicht LH (1993) Regulated expression of an intestinal mucin gene in HT29 colonic carcinoma cells. J Biol Chem 268:13956–13961
Weinstein LS, Yu S, Warner DR, Liu J (2001) Endocrine manifestations of stimulatory G protein alpha-subunit mutations and the role of genomic imprinting. Endocr Rev 22:675–705. https://doi.org/10.1210/edrv.22.5.0439
Wu J et al (2011) Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci Transl Med 3:92ra66. https://doi.org/10.1126/scitranslmed.3002543
Yan FC, Li XB, Lin YL, Yu CK, Zhou Q, Li Y (2019) Clinicopathological analysis of ovarian pseudomyxoma peritonei Chin. J Clin Oncol 46:887–890
Yan FC, Lin YL, Zhou Q, Chang H, Li Y (2020) Pathological prognostic factors of pseudomyxoma peritonei: comprehensive clinicopathological analysis of 155 cases. Hum Pathol. https://doi.org/10.1016/j.humpath.2019.12.008
Acknowledgements
Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20180701); Special Fund for the Capital Characteristic Clinical Medicine Development Project (Z161100000516077); Beijing Municipal Grant for Medical Talents Group on Peritoneal Surface Oncology (2017400003235J007); Key Discipline Development Fund of Beijing Shijitan Hospital, Capital Medical University (2016fmzlwk); Beijing Natural Science Foundation (7172108); Beijing Health and Science Technology Achievement and Appropriate Technology Promotion Project (2018-TG-27).
Funding
This study was supported by funding from Beijing Municipal Administration of Hospitals’ Ascent Plan (DFL20180701); Special Fund for the Capital Characteristic Clinical Medicine Development Project, Beijing Municipal Science and Technology Commission (Z161100000516077); Beijing Municipal Grant for Medical Talents Group on Peritoneal Surface Oncology (2017400003235J007); Key Discipline Development Fund of Beijing Shijitan Hospital, Capital Medical University (2016fmzlwk); Beijing Natural Science Foundation (7172108); Beijing Health and Science Technology Achievement and Appropriate Technology Promotion Project (2018-TG-27).
Author information
Authors and Affiliations
Contributions
Y-LL was responsible for literature review, data collection and analysis, summary, and manuscript writing; RM helped to summarize tables and revise/review manuscript; YL designed the study and refined manuscript definition of intellectual content. Manuscript of final version was approved by YL.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, YL., Ma, R. & Li, Y. The biological basis and function of GNAS mutation in pseudomyxoma peritonei: a review. J Cancer Res Clin Oncol 146, 2179–2188 (2020). https://doi.org/10.1007/s00432-020-03321-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-020-03321-8