Abstract
Background
The management of intraductal papillary mucinous neoplasms (IPMNs) is mainly based on imaging features and clinical symptoms, and remains challenging.
Objective
The aim of this study was to assess GNAS, RAS family (KRAS, NRAS and HRAS), BRAF, and PIK3CA mutation status in resected IPMNs and correlate it with clinicopathological characteristics and patient survival.
Methods
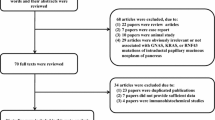
Overall, 149 consecutive unselected patients who underwent pancreatectomy for IPMNs were included. After dissection from formalin-fixed and paraffin-embedded tumors, GNAS mutational screening was assessed by allelic discrimination using Taqman® probes and confirmed by SNaPshot analysis. RAS family, BRAF, and PIK3CA mutational screening was assessed by high resolution melt and Sanger sequencing.
Results
Gastric- and intestinal-type IPMNs were the most frequent lesions (52% and 41%, respectively). Intestinal-type IPMNs were more frequently associated high-grade dysplasia (49%) and were the only IPMNs associated with colloid-type carcinoma. All pancreatobiliary IPMNs were invasive lesions, located in the main pancreatic duct. GNAS-activating mutations were strongly associated with the intestinal phenotype (p < 10−4), while RAS pathway mutations were not associated with any particular phenotype. Mutations within other members of the epidermal growth factor receptor (EGFR) pathway were very rare (2%). GNAS-mutated IPMNs were rarely invasive (11%) and almost exclusively (83%) of the colloid type. For invasive lesions, multivariate analyses determined that only node negativity was associated with improved cancer-specific survival, but, in univariate analysis, GNAS mutation was associated with prolonged survival.
Conclusion
In patients selected for surgery, GNAS mutation analysis and tumor phenotype can help to better predict patient prognosis. In the near future, a more precise mutational analysis of IPMNs might help to better tailor their management.



Similar content being viewed by others
References
Distler M, Kersting S, Niedergethmann M, et al. Pathohistological subtype predicts survival in patients with intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann Surg. 2013; 258(2):324–30.
Furukawa T, Hatori T, Fujita I, et al. Prognostic relevance of morphological types of intraductal papillary mucinous neoplasms of the pancreas. Gut. 2011; 60(4):509–16.
European Study Group on Cystic Tumours of the P. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67(5):789–804.
Tanaka M, Fernandez-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17(5):738–753.
Marchegiani G, Mino-Kenudson M, Ferrone CR, et al. Patterns of recurrence after resection of IPMN: who, when, and how? Ann Surg. 2015; 262(6):1108–14.
Lawrence SA, Attiyeh MA, Seier K, et al. Should patients with cystic lesions of the pancreas undergo long-term radiographic surveillance?: Results of 3024 patients evaluated at a single institution. Ann Surg. 2017; 266(3):536–544.
Wu J, Matthaei H, Maitra A, et al. Recurrent GNAS mutations define an unexpected pathway for pancreatic cyst development. Sci Transl Med. 2011; 3(92):92ra66.
Wu J, Jiao Y, Dal Molin M, et al. Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways. Proc Natl Acad Sci U S A. 2011; 108(52):21188–93.
Kanda M, Knight S, Topazian M, et al. Mutant GNAS detected in duodenal collections of secretin-stimulated pancreatic juice indicates the presence or emergence of pancreatic cysts. Gut. 2012; 62:1024–33.
Furukawa T, Kuboki Y, Tanji E, et al. Whole-exome sequencing uncovers frequent GNAS mutations in intraductal papillary mucinous neoplasms of the pancreas. Sci Rep. 2011; 1:161.
Weinstein LS, Shenker A, Gejman PV, et al. Activating mutations of the stimulatory G protein in the McCune-Albright syndrome. N Engl J Med. 1991; 325(24):1688–95.
Dal Molin M, Matthaei H, Wu J, et al. Clinicopathological correlates of activating GNAS mutations in intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Ann Surg Oncol. 2013; 20:3802–8.
Kanda M, Knight S, Topazian M, et al. Mutant GNAS detected in duodenal collections of secretin-stimulated pancreatic juice indicates the presence or emergence of pancreatic cysts. Gut. 2013; 62(7):1024–33.
Singhi AD, McGrath K, Brand RE, et al. Preoperative next-generation sequencing of pancreatic cyst fluid is highly accurate in cyst classification and detection of advanced neoplasia. Gut. 2017; 67:2131–41.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6(1–2):17–32.
Tanaka M, Fernandez-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012; 12(3):183–97.
Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004; 28(8):977–87.
Basturk O, Hong SM, Wood LD, et al. A revised classification system and recommendations from the baltimore consensus meeting for neoplastic precursor lesions in the pancreas. Am J Surg Pathol. 2015; 39(12):1730–41.
Nara S, Shimada K, Kosuge T, et al. Minimally invasive intraductal papillary-mucinous carcinoma of the pancreas: clinicopathologic study of 104 intraductal papillary-mucinous neoplasms. Am J Surg Pathol. 2008; 32(2):243–55.
Parvanescu A, Cros J, Ronot M, et al. Lessons from McCune-Albright syndrome-associated intraductal papillary mucinous neoplasms:: GNAS-activating mutations in pancreatic carcinogenesis. JAMA Surg. 2014; 149(8):858–62.
Cacheux W, Rouleau E, Briaux A, et al. Mutational analysis of anal cancers demonstrates frequent PIK3CA mutations associated with poor outcome after salvage abdominoperineal resection. Br J Cancer. 2016; 114(12):1387–94.
Mino-Kenudson M, Fernandez-del Castillo C, Baba Y, et al. Prognosis of invasive intraductal papillary mucinous neoplasm depends on histological and precursor epithelial subtypes. Gut. 2011; 60(12):1712–20.
Nakata K, Ohuchida K, Aishima S, et al. Invasive carcinoma derived from intestinal-type intraductal papillary mucinous neoplasm is associated with minimal invasion, colloid carcinoma, and less invasive behavior, leading to a better prognosis. Pancreas. 2011; 40(4):581–7.
Tan MC, Basturk O, Brannon AR, et al. GNAS and KRAS mutations define separate progression pathways in intraductal papillary mucinous neoplasm-associated carcinoma. J Am Coll Surg. 2015; 220(5):845–54 e1.
Adsay NV, Merati K, Basturk O, et al. Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol. 2004; 28(7):839–48.
Kuboki Y, Shimizu K, Hatori T, et al. Molecular biomarkers for progression of intraductal papillary mucinous neoplasm of the pancreas. Pancreas. 2015; 44(2):227–35.
Innamorati G, Valenti MT, Giacomello L, et al. GNAS mutations: drivers or co-pilots? Yet, promising diagnostic biomarkers. Trends Cancer. 2016; 2(6):282–5.
Taki K, Ohmuraya M, Tanji E, et al. GNAS(R201H) and Kras(G12D) cooperate to promote murine pancreatic tumorigenesis recapitulating human intraductal papillary mucinous neoplasm. Oncogene. 2016; 35(18):2407–12.
Komatsu H, Tanji E, Sakata N, et al. A GNAS mutation found in pancreatic intraductal papillary mucinous neoplasms induces drastic alterations of gene expression profiles with upregulation of mucin genes. PLoS ONE. 2014; 9(2):e87875.
Felsenstein M, Noe M, Masica DL, et al. IPMNs with co-occurring invasive cancers: neighbours but not always relatives. Gut. 2018; 67:1652–62.
Omori Y, Ono Y, Tanino M, et al. Pathways of progression from intraductal papillary mucinous neoplasm to pancreatic ductal adenocarcinoma based on molecular features. Gastroenterology. 2019; 156(3):647–61 e2.
Chang YR, Park JK, Jang JY, et al. Incidental pancreatic cystic neoplasms in an asymptomatic healthy population of 21,745 individuals: large-scale, single-center cohort study. Medicine (Baltimore). 2016; 95(51):e5535.
Falconi M, Crippa S, Chari S, et al. Quality assessment of the guidelines on cystic neoplasms of the pancreas. Pancreatology. 2015; 15(5):463–9.
Marchegiani G, Andrianello S, Borin A, et al. Systematic review, meta-analysis, and a high-volume center experience supporting the new role of mural nodules proposed by the updated 2017 international guidelines on IPMN of the pancreas. Surgery. 2018; 163(6):1272–9.
Springer S, Wang Y, Dal Molin M, et al. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Gastroenterology. 2015; 149(6):1501–10.
Yoon WJ, Brugge WR. The safety of endoscopic ultrasound-guided fine-needle aspiration of pancreatic cystic lesions. Endosc Ultrasound. 2015; 4(4):289–92.
Mori Y, Ohtsuka T, Kono H, et al. A minimally invasive and simple screening test for detection of pancreatic ductal adenocarcinoma using biomarkers in duodenal juice. Pancreas. 2013; 42(2):187–92.
Berger AW, Schwerdel D, Costa IG, et al. Detection of hot-spot mutations in circulating cell-free DNA from patients with intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology. 2016; 151(2):267–70.
Crippa S, Bassi C, Salvia R, et al. Low progression of intraductal papillary mucinous neoplasms with worrisome features and high-risk stigmata undergoing non-operative management: a mid-term follow-up analysis. Gut. 2017; 66(3):495–506.
Acknowledgment
The authors would like to thank Walid Chemlali for technical assistance, and all the Beaujon and Cochin clinical and technical staff for their helpful discussions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sébastien Gaujoux, Alina Parvanescu, Manuella Cesaretti, Caroline Silve, Ivan Bieche, Vinciane Rebours, Philippe Lévy, Alain Sauvanet, and Jérôme Cros have no financial or personal conflicts of interest in relation to this study.
Funding
This work was supported by Fonds d’Aide à la Recherche et à l’Evaluation (FARE) from the Société Nationale Française de Gastro-entérologie (SNFGE).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gaujoux, S., Parvanescu, A., Cesaretti, M. et al. GNAS but Not Extended RAS Mutations Spectrum are Associated with a Better Prognosis in Intraductal Pancreatic Mucinous Neoplasms. Ann Surg Oncol 26, 2640–2650 (2019). https://doi.org/10.1245/s10434-019-07389-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07389-6